Intro
I work with stem cells in the lab, so I want to share the information on that topic at that blog. There are lots of interesting articles and study materials about stem cells on the web that's why I'm trying to gather them all here.
12/29/2011
12/27/2011
Stem Cells!
Beautiful Stem Cells! Thnx to
http://stemcelldaily.com/stem-cells-are-purdy-pics/ :

Neurosphere composed of neural precursor cells as captured by a fluorescent microscope. The cells, allowed to attach to a substrate, have begun to send out long processes that will eventually become the axons of the mature neurons.
The image was taken in the lab of Martin Pera at the University of Southern California.

A confocal microscopic image of a neurosphere, a ball of human embryonic stem cells giving rise to nerve cells. The nuclei of the neurons are shown in blue, while the axons are shown in red.
The image was taken in the lab of Juan Carlos Izpisua Belmonte at The Salk Institute for Biological Studies.

Color-enhanced electron microscopic image of mouse embryonic stem cells growing on a bed of silicon nanotubes.
The image was taken in the lab of Bruce Conklin at the Gladstone Institute for Cardiovascular Medicine.

Color-enhanced image taken by a scanning electron microscope of retinal pigment epithelial (RPE) cells derived from human embryonic stem cells. The cells are remarkably similar to normal RPE cells, having a hexagonal shape and growing in a single, well defined layer. These cells are the ones responsible for macular degeneration, the most common cause of blindness. CIRM scientists hope to one day treat macular degeneration with transplanted RPE cells derived from human embryonic stem cells.
The image was taken in the lab of David Hinton at the University of Southern California.
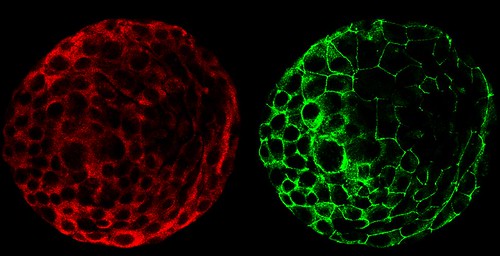

A composite of two images taken of a human embryo under different fluorescent wavelengths using a confocal microscope.
Fluorescent tags reveal that cells on the surface of the embryo are expressing human chorinoic gonadotropin (green tag) and an adhesion molecule (red tag)that helps them stick together.
The image was taken in the lab of Susan Fisher at the University of California, San Francisco.
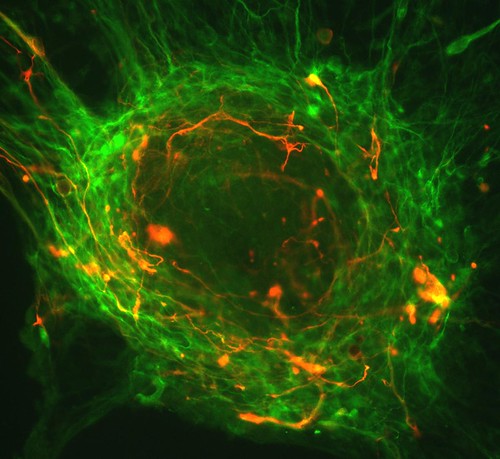

A fluorescent microscopic image of hundreds of human embryonic stem cells in various stages of differentiation into neurons. Some cells have become neurons (red), while others are still precursors of nerve cells (green). The yellow is an imaging artifact that results when cells in both stages are on top of each other.
The image was taken in the lab of Guoping Fan at the University of California, Los Angeles.

Colonies of human embryonic stem cells as seen with a fluorescent microscope. Nuclei have been stained blue, while regions that appear pink and green have been stained with antibodies, indicating the cells’ pluripotency — that unique ability of stem cells to differentiate into a variety of cell types.
The image was taken in the lab of Prue Talbot at the University of California, Riverside.


Three neurons (red) derived from human embryonic stem cells (hESCs) as seen by a confocal microscope. Visible are neural cell bodies, complete with axons and dendrites (red), used for cell-to-cell communications, as well as undifferentiated hESCs (green).
The image was taken in the lab of Anirvan Ghosh at the University of California, San Diego.


A fluorescent microscopic image of a functional neuron with an axon (red) growing above the cell’s nucleus and three dendrites (red) below. Undifferentiated neural precursor cells (blue) are visible as are glia cells (green) that have differentiated from the same group of mouse neural stem cells.
The image was taken in the lab of Paul Knoepfler at the University of California, Davis.


Two neurospheres, compact masses of neuron precursor cells, derived from human embryonic stem cells, as captured by a fluorescent microscope. Differentiated neurons, whose nuclei are shown in red, have begun to extend neuronal processes (green) toward one another, forming connections.

Neurosphere composed of neural precursor cells as captured by a fluorescent microscope. The cells, allowed to attach to a substrate, have begun to send out long processes that will eventually become the axons of the mature neurons.
The image was taken in the lab of Martin Pera at the University of Southern California.

A confocal microscopic image of a neurosphere, a ball of human embryonic stem cells giving rise to nerve cells. The nuclei of the neurons are shown in blue, while the axons are shown in red.
The image was taken in the lab of Juan Carlos Izpisua Belmonte at The Salk Institute for Biological Studies.

Color-enhanced electron microscopic image of mouse embryonic stem cells growing on a bed of silicon nanotubes.
The image was taken in the lab of Bruce Conklin at the Gladstone Institute for Cardiovascular Medicine.

Color-enhanced image taken by a scanning electron microscope of retinal pigment epithelial (RPE) cells derived from human embryonic stem cells. The cells are remarkably similar to normal RPE cells, having a hexagonal shape and growing in a single, well defined layer. These cells are the ones responsible for macular degeneration, the most common cause of blindness. CIRM scientists hope to one day treat macular degeneration with transplanted RPE cells derived from human embryonic stem cells.
The image was taken in the lab of David Hinton at the University of Southern California.
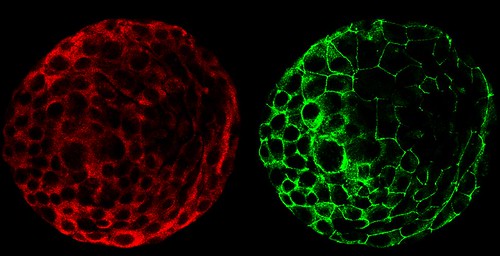

A composite of two images taken of a human embryo under different fluorescent wavelengths using a confocal microscope.
Fluorescent tags reveal that cells on the surface of the embryo are expressing human chorinoic gonadotropin (green tag) and an adhesion molecule (red tag)that helps them stick together.
The image was taken in the lab of Susan Fisher at the University of California, San Francisco.
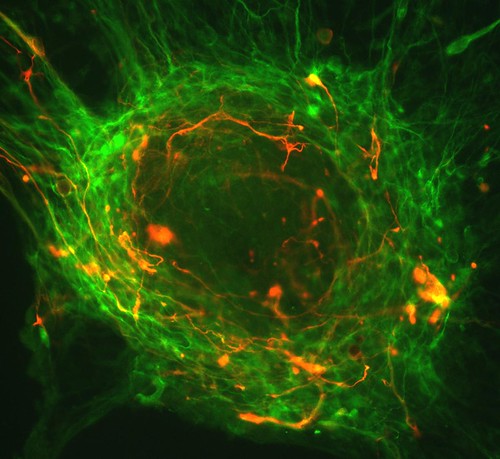

A fluorescent microscopic image of hundreds of human embryonic stem cells in various stages of differentiation into neurons. Some cells have become neurons (red), while others are still precursors of nerve cells (green). The yellow is an imaging artifact that results when cells in both stages are on top of each other.
The image was taken in the lab of Guoping Fan at the University of California, Los Angeles.

Colonies of human embryonic stem cells as seen with a fluorescent microscope. Nuclei have been stained blue, while regions that appear pink and green have been stained with antibodies, indicating the cells’ pluripotency — that unique ability of stem cells to differentiate into a variety of cell types.
The image was taken in the lab of Prue Talbot at the University of California, Riverside.


Three neurons (red) derived from human embryonic stem cells (hESCs) as seen by a confocal microscope. Visible are neural cell bodies, complete with axons and dendrites (red), used for cell-to-cell communications, as well as undifferentiated hESCs (green).
The image was taken in the lab of Anirvan Ghosh at the University of California, San Diego.


A fluorescent microscopic image of a functional neuron with an axon (red) growing above the cell’s nucleus and three dendrites (red) below. Undifferentiated neural precursor cells (blue) are visible as are glia cells (green) that have differentiated from the same group of mouse neural stem cells.
The image was taken in the lab of Paul Knoepfler at the University of California, Davis.


Two neurospheres, compact masses of neuron precursor cells, derived from human embryonic stem cells, as captured by a fluorescent microscope. Differentiated neurons, whose nuclei are shown in red, have begun to extend neuronal processes (green) toward one another, forming connections.
The image was taken in the lab of Fred H. Gage at the Salk Institute for Biological Studies.

Neurospheres made up of neural stem cells derived from human embryonic stem cells captured using fluorescence microscopy. Some cells (green) are destined to become neurons; others have yet to differentiate (red) or are in transition (yellow).
This photo was taken in the lab of Brian Cummings at the University of California, Irvine.

A composite image of frames taken of a developing human embryo captured using time-lapse video microscopy and a phase contrast microscope. The earliest frame is of a three-day-old embryo and appears in the upper left corner. An image of a five-day-old embryo appears in the lower right.
This photo was taken in the lab of Susan Fisher at the University of California, San Francisco.
You can find out more information about the contest here.

Neurospheres made up of neural stem cells derived from human embryonic stem cells captured using fluorescence microscopy. Some cells (green) are destined to become neurons; others have yet to differentiate (red) or are in transition (yellow).
This photo was taken in the lab of Brian Cummings at the University of California, Irvine.

A composite image of frames taken of a developing human embryo captured using time-lapse video microscopy and a phase contrast microscope. The earliest frame is of a three-day-old embryo and appears in the upper left corner. An image of a five-day-old embryo appears in the lower right.
This photo was taken in the lab of Susan Fisher at the University of California, San Francisco.
You can find out more information about the contest here.
Stem Cells Can Kill Rare genetic Skin Disease
John E. Wagner and Jakub Tolar, in collaboration with researchers in Portland, Oregon, the United Kingdom, and Japan have for the first time used stem cells from bone marrow to repair the skin of patients with a fatal skin disease called recessive dystrophic epidermolysis bullosa, or RDEB.
This is the first time researchers have shown that bone marrow stem cells can home to the skin and upper gastrointestinal tract and alter the natural course of the disease.
"Whether stem cells from marrow could repair tissues other than itself has been quite controversial," said Wagner.
"But in 2007 we found a rare subpopulation of marrow stem cells that could repair the skin in laboratory models. This astounding finding compelled us to test these stem cells in humans. This has never been done before," Wagner added.
Tolar said: "This discovery is more unique and more remarkable than it may first soundbecause until now, bone marrow has only been used to replace diseased or damaged marrow – which makes sense.
"But what we have found is that stem cells contained in bone marrow can travel to sites of injured skin, leading to increased production of collagen which is deficient in patients with RDEB," Tolar added.
Epidermolysis bullosa (EB) is a rare, genetic skin disease that causes skin to blister and scrape off with the slightest friction or trauma. It affects the skin and lining of the mouth and esophagus. Previously, there was no treatment and no chance for cure.
In some countries, even euthanasia has been considered for newborns with the severest forms. If children with EB do not die of infection in their early life, many with the disease do not live beyond their 20s or 30s because they develop an aggressive form of skin cancer. While a few will live long term, the severest forms of EB are generally lethal.
"Bone marrow transplantation is one of the riskiest procedures in medicine, yet it is also one of the most successful. Patients who otherwise would have died from their disease can often now be cured. It''s a serious treatment for a serious disease," said Tolar. (ANI)
This is the first time researchers have shown that bone marrow stem cells can home to the skin and upper gastrointestinal tract and alter the natural course of the disease.
"Whether stem cells from marrow could repair tissues other than itself has been quite controversial," said Wagner.
"But in 2007 we found a rare subpopulation of marrow stem cells that could repair the skin in laboratory models. This astounding finding compelled us to test these stem cells in humans. This has never been done before," Wagner added.
Tolar said: "This discovery is more unique and more remarkable than it may first soundbecause until now, bone marrow has only been used to replace diseased or damaged marrow – which makes sense.
"But what we have found is that stem cells contained in bone marrow can travel to sites of injured skin, leading to increased production of collagen which is deficient in patients with RDEB," Tolar added.
Epidermolysis bullosa (EB) is a rare, genetic skin disease that causes skin to blister and scrape off with the slightest friction or trauma. It affects the skin and lining of the mouth and esophagus. Previously, there was no treatment and no chance for cure.
In some countries, even euthanasia has been considered for newborns with the severest forms. If children with EB do not die of infection in their early life, many with the disease do not live beyond their 20s or 30s because they develop an aggressive form of skin cancer. While a few will live long term, the severest forms of EB are generally lethal.
"Bone marrow transplantation is one of the riskiest procedures in medicine, yet it is also one of the most successful. Patients who otherwise would have died from their disease can often now be cured. It''s a serious treatment for a serious disease," said Tolar. (ANI)
Human Breast Stem Cells
Adult human breast stem cells (red) are found in ductal regions. Lineage-restricted progenitor cell types (green) reside outside ducts in lobules. (JCB 177(1) TOC2)
Equal survival rates between two major sources of blood cells.
Interesting news...
Patients who receive a blood stem cell transplant from a donor outside of their family to treatleukemia and other blood diseases are more likely to have graft failure but less likely to experience graft-versus-host disease, a condition caused by the donor cells attacking the recipient’s body, if the transplanted blood cells come directly from a donor’s bone marrow, rather than from blood stem cells circulating in the donor’s bloodstream (PBSCs), according to new research. Although the study showed differences in the type and extent of complications, the results showed no difference in patient survival rates between these two major sources of donated blood cells.
Patients who receive a blood stem cell transplant from a donor outside of their family to treatleukemia and other blood diseases are more likely to have graft failure but less likely to experience graft-versus-host disease, a condition caused by the donor cells attacking the recipient’s body, if the transplanted blood cells come directly from a donor’s bone marrow, rather than from blood stem cells circulating in the donor’s bloodstream (PBSCs), according to new research. Although the study showed differences in the type and extent of complications, the results showed no difference in patient survival rates between these two major sources of donated blood cells.
Another one doubt...
High-dose chemotherapy and autologous stem cell transplantation (HDC-ASCT), for previously untreated patients with advanced follicular lymphoma (FL) does not improve overall survival compared with conventional-dose chemotherapy alone, according to an online study published December 21 in the Journal of the National Cancer Institute.
12/26/2011
In vivo clonal analysis reveals self-renewing and multipotent adult neural stem cell characteristics
New information from http://www.stemcellspuhua.com/r292.html
2011, by by Michael A Bonaguidi, Michael A Wheeler, Jason S Shapiro, Ryan P Stadel, Gerald J Sun, Guo-li Ming, Hongjun Song
Neurogenesis and gliogenesis continue in discrete regions of the adult mammalian brain. A fundamental question remains whether cell genesis occurs from distinct lineage-restricted progenitors or from self-renewing and multipotent neural stem cells in the adult brain. Here, we developed a genetic marking strategy for lineage tracing of individual, quiescent, and nestin-expressing radial glia-like (RGL) precursors in the adult mouse dentate gyrus. Clonal analysis identified multiple modes of RGL activation, including asymmetric and symmetric self-renewal. Long-term lineage tracing invivo revealed a significant percentage of clones that contained RGL(s), neurons, and astrocytes, indicating capacity of individual RGLs for both self-renewal and multilineage differentiation. Furthermore, conditional Pten deletion in RGLs initially promotes their activation and symmetric self-renewal but ultimately leads to terminal astrocytic differentiation and RGL depletion in the adult hippocampus. Our study identifies RGLs as self-renewing and multipotent neural stem cells and provides novel insights into invivo properties of adult neural stem cells.
Available from www.ncbi.nlm.nih.gov
Stem Cell SPIONs
SPIONs for Stem cell therapy! Check it out at
http://www.stemcellresearchnews.com/absolutenm/anmviewer.asp?a=2769&z=9
In a discovery that may help speed use of cell therapy, scientists report development of a way to deliver therapeutic human cells to diseased areas within the body using a simple magnetic effect.
Rawil Fakhrullin and colleagues from the Kazan State Medical University (Republic of Tatarstan) said that cell therapy aims to replace damaged or diseased cells in the human body with normal cells or stem cells. To do so, medical personnel need a way to target these cells to diseased organs or tissues.
So-called superparamagnetic iron oxide nanoparticles (SPIONs), attached to therapeutic cells, show promise. Magnetic devices could be used to move such cells to diseased areas of the body. But current ways of attaching SPIONs to therapeutic cells are difficult to use and may damage the therapeutic cells. So the researchers set out to develop a better process for attaching SPIONs to human cells.
They describe a new process for making “stabilized” SPIONs in the laboratory and successful attachment of these magnetic nanoparticles to the outside of human cells.
They found that the SPIONs were not toxic to cells, and they moved in response to a magnet.
“Our current results, as we believe, will inspire scientists to apply the simple and direct technique reported here in tissue engineering and cell-based therapies,” the researchers wrote.
Citation: “A Direct Technique for Magnetic Functionalization of Living Human Cells;” Maria R. Dzamukova, Rawil Fakhrullin et al.; Langmuir, 27 October 2011, 27 (23), pp 14386–14393, DOI: 10.1021/la203839v
Abstract: Click here.
Contact: Rawil Fakhrullin, +7-843-233-78-33,kazanbio@gmail.com
In a discovery that may help speed use of cell therapy, scientists report development of a way to deliver therapeutic human cells to diseased areas within the body using a simple magnetic effect.
Rawil Fakhrullin and colleagues from the Kazan State Medical University (Republic of Tatarstan) said that cell therapy aims to replace damaged or diseased cells in the human body with normal cells or stem cells. To do so, medical personnel need a way to target these cells to diseased organs or tissues.
So-called superparamagnetic iron oxide nanoparticles (SPIONs), attached to therapeutic cells, show promise. Magnetic devices could be used to move such cells to diseased areas of the body. But current ways of attaching SPIONs to therapeutic cells are difficult to use and may damage the therapeutic cells. So the researchers set out to develop a better process for attaching SPIONs to human cells.
They describe a new process for making “stabilized” SPIONs in the laboratory and successful attachment of these magnetic nanoparticles to the outside of human cells.
They found that the SPIONs were not toxic to cells, and they moved in response to a magnet.
“Our current results, as we believe, will inspire scientists to apply the simple and direct technique reported here in tissue engineering and cell-based therapies,” the researchers wrote.
Citation: “A Direct Technique for Magnetic Functionalization of Living Human Cells;” Maria R. Dzamukova, Rawil Fakhrullin et al.; Langmuir, 27 October 2011, 27 (23), pp 14386–14393, DOI: 10.1021/la203839v
Abstract: Click here.
Contact: Rawil Fakhrullin, +7-843-233-78-33,kazanbio@gmail.com
Embryonic stem cell
Isn't it gorgeous? :)
B0006219 Human embryonic stem cell
Credit: Annie Cavanagh. Wellcome Images
images@wellcome.ac.uk
http://images.wellcome.ac.uk
Copyrighted work available under Creative Commons by-nc-nd 2.0 UK, see http://images.wellcome.ac.uk/indexplus/page/Prices.html
B0006219 Human embryonic stem cell
Credit: Annie Cavanagh. Wellcome Images
images@wellcome.ac.uk
http://images.wellcome.ac.uk
Copyrighted work available under Creative Commons by-nc-nd 2.0 UK, see http://images.wellcome.ac.uk/indexplus/page/Prices.html
FT1050 - new compound for stem cell therapies
http://www.sciencedaily.com/releases/2011/12/111212220942.htm:
ScienceDaily (Dec. 12, 2011) — A therapy involving a natural compound may improve the ability of stem cells from umbilical cord blood to engraft in patients receiving a stem cell transplant for cancer or other diseases, a phase I clinical trial led by Dana-Farber Cancer Institute scientists indicates.
"There is a significant need to improve the speed and quality of engraftment of cord-derived stem cells," says trial leader Corey Cutler, MD, MPH, of Dana-Farber and Brigham and Women's Hospital. "FT1050 has shown the ability in preclinical research to activate hematopoetic [blood-forming] stem cells so they engraft more quickly and with a higher degree of success."
FT1050-treated blood-forming stem cells are being tested as a possible solution to one of the major shortcomings of transplants involving stem cells from umbilical cord blood: the relatively small number of stem cells infused in such procedures often take longer to engraft -- or take root -- in patients than do the more numerous stem cells involved in transplants from adult donors. The delay can leave patients susceptible to dangerous infections and other complications.
Umbilical cord stem cell transplants are an option for patients who do not have a closely-matched adult donor. Because the current pool of potential donors is smaller for non-Caucasians than for Caucasians, members of ethnic minorities tend to receive transplants from cord blood at a higher rate than Caucasians do.
The goal of the phase I trial was to assess the safety of FT1050-treated cord blood cells in adult patients receiving umbilical cord blood stem cell transplants, and determine if the treated cells accelerate engraftment. In the 12 patients who participated in the trial, engraftment occurred approximately three to four days faster than happens with standard cord blood cells. Levels of white blood cells known as neutrophils returned to normal in the patients after a median of 17.5 days, similar to the rate in standard stem cell transplants. Side effects of the FT1050-treated cord blood cells were minimal. In none of the study patients did the stem cells fail to engraft.
The phase I trial was sponsored by Fate Therapeutics, Inc., of San Diego, Calif., which is developing ProHema, a biologic product consisting of hematopoietic stem cells treated with FT1050 for patients undergoing stem cell transplantation. FT1050 was identified by Leonard Zon, MD, a hematologist and director of the Stem Cell Program at Children's Hospital Boston, using chemical screens conducted in zebrafish, and is the first potential therapeutic derived from a zebrafish model to make into clinical trials.
"We're encouraged by the results of this study for patients receiving umbilical cord stem cell transplants after reduced-intensity chemotherapy treatment," Cutler says. "Further studies are planned to test FT1050-treated hematopoietic stem cells in a larger group of these patients."
ScienceDaily (Dec. 12, 2011) — A therapy involving a natural compound may improve the ability of stem cells from umbilical cord blood to engraft in patients receiving a stem cell transplant for cancer or other diseases, a phase I clinical trial led by Dana-Farber Cancer Institute scientists indicates.
"There is a significant need to improve the speed and quality of engraftment of cord-derived stem cells," says trial leader Corey Cutler, MD, MPH, of Dana-Farber and Brigham and Women's Hospital. "FT1050 has shown the ability in preclinical research to activate hematopoetic [blood-forming] stem cells so they engraft more quickly and with a higher degree of success."
FT1050-treated blood-forming stem cells are being tested as a possible solution to one of the major shortcomings of transplants involving stem cells from umbilical cord blood: the relatively small number of stem cells infused in such procedures often take longer to engraft -- or take root -- in patients than do the more numerous stem cells involved in transplants from adult donors. The delay can leave patients susceptible to dangerous infections and other complications.
Umbilical cord stem cell transplants are an option for patients who do not have a closely-matched adult donor. Because the current pool of potential donors is smaller for non-Caucasians than for Caucasians, members of ethnic minorities tend to receive transplants from cord blood at a higher rate than Caucasians do.
The goal of the phase I trial was to assess the safety of FT1050-treated cord blood cells in adult patients receiving umbilical cord blood stem cell transplants, and determine if the treated cells accelerate engraftment. In the 12 patients who participated in the trial, engraftment occurred approximately three to four days faster than happens with standard cord blood cells. Levels of white blood cells known as neutrophils returned to normal in the patients after a median of 17.5 days, similar to the rate in standard stem cell transplants. Side effects of the FT1050-treated cord blood cells were minimal. In none of the study patients did the stem cells fail to engraft.
The phase I trial was sponsored by Fate Therapeutics, Inc., of San Diego, Calif., which is developing ProHema, a biologic product consisting of hematopoietic stem cells treated with FT1050 for patients undergoing stem cell transplantation. FT1050 was identified by Leonard Zon, MD, a hematologist and director of the Stem Cell Program at Children's Hospital Boston, using chemical screens conducted in zebrafish, and is the first potential therapeutic derived from a zebrafish model to make into clinical trials.
"We're encouraged by the results of this study for patients receiving umbilical cord stem cell transplants after reduced-intensity chemotherapy treatment," Cutler says. "Further studies are planned to test FT1050-treated hematopoietic stem cells in a larger group of these patients."
Pigs are our friends :)
Pig stem cell research conducted by two animal scientists at the University of Georgia reveals a better way to determine the safety of future stem cell therapies than rodent-based models.
Rodent studies are likely inadequate for testing many human therapies - including pharmaceuticals - since 50 percent of all chemicals test positive as carcinogens in rodents regardless of their source or identity, according to Thomas Hartung, a professor in the Bloomsburg College of Public Health at Johns Hopkins University. He suggests these rodent studies may be no better than a coin toss. For example, some components in coffee appear to be carcinogenic in rodents, but in humans moderate coffee consumption may reduce the risk of cancer.
In 2010, UGA faculty Steve Stice and Franklin West introduced 13 pigs that have shown promise in unlocking the path to new therapies. The pigs recently produced another positive finding: These adult-cell-sourced stem cells don't form tumors in pigs.
"Pluripotent stem cells have significant potential for stem cell therapies," said West, an animal science researcher and assistant professor in the UGA College of Agricultural and Environmental Sciences. "However, tests in mice often resulted in tumor formation that frequently led to death."
The formation of tumors has raised concerns about the safety of induced pluripotent stem cells, or iPSCs, and cells derived from these stem cells. Until now, all iPSC safety studies have been performed in rodent models.
"To address the concern, our research team studied tumor formation in pigs generated from pig iPSCs," West said. "Brain, skin, liver, pancreas, stomach, intestine, lung, heart, kidney, muscle, spleen and gonad tissues from all 11 pigs tested showed no evidence of tumors."
The absence of tumor formation in these pigs suggests that iPSCs can safely incorporate into tissues without tumor formation.
"Being able to safely use iPSCs without the potential of causing tumors is essential for this promising stem cell therapy to become a viable treatment option," said Stice, a Georgia Research Alliance Eminent Scholar in the College of Agricultural and Environmental Sciences. "We now have graduate students working on making neural cells from the human and pig stem cells to help further the studies. The human stem cells were effective in a rodent model for stroke, but rodent studies are not rigorous enough to start human clinical trials."
West agrees. "Over 700 drug treatments have gone to human clinical trials for stroke alone based on findings in rodents and have turned out not to be viable in humans," he said. "The pigs are much more human like, and they are going to be a much better model to study strokes."
West is leading a cooperative project between the UGA Regenerative Bioscience Center and stroke researchers at Georgia Health Sciences University. "This project will improve the speed and efficiency of treatment development for stroke and many other conditions and potentially reduce the number of nonhuman primates used in research," he said.
Additionally, Stice and West have now bred the pigs produced from iPSCs and have proven the stem cells did pass to the offspring. This finding opens the door for better animal-sourced tissue for human regenerative medicine such as islet cells that produce insulin for diabetic patients.
Using iPSC technology, the UGA Regenerative Bioscience Center is working with researchers at Emory University to make pigs whose cells from the pancreas would demonstrate decreased rejection in human treatments.
"The next step would be to put these pig insulin-producing cells into other animals, potentially dogs or cats suffering from diabetes - to see if it will produce insulin for them without being rejected," Stice said. "So, it's moving forward. Never as fast as we like, but it's moving."
Rodent studies are likely inadequate for testing many human therapies - including pharmaceuticals - since 50 percent of all chemicals test positive as carcinogens in rodents regardless of their source or identity, according to Thomas Hartung, a professor in the Bloomsburg College of Public Health at Johns Hopkins University. He suggests these rodent studies may be no better than a coin toss. For example, some components in coffee appear to be carcinogenic in rodents, but in humans moderate coffee consumption may reduce the risk of cancer.
In 2010, UGA faculty Steve Stice and Franklin West introduced 13 pigs that have shown promise in unlocking the path to new therapies. The pigs recently produced another positive finding: These adult-cell-sourced stem cells don't form tumors in pigs.
"Pluripotent stem cells have significant potential for stem cell therapies," said West, an animal science researcher and assistant professor in the UGA College of Agricultural and Environmental Sciences. "However, tests in mice often resulted in tumor formation that frequently led to death."
The formation of tumors has raised concerns about the safety of induced pluripotent stem cells, or iPSCs, and cells derived from these stem cells. Until now, all iPSC safety studies have been performed in rodent models.
"To address the concern, our research team studied tumor formation in pigs generated from pig iPSCs," West said. "Brain, skin, liver, pancreas, stomach, intestine, lung, heart, kidney, muscle, spleen and gonad tissues from all 11 pigs tested showed no evidence of tumors."
The absence of tumor formation in these pigs suggests that iPSCs can safely incorporate into tissues without tumor formation.
"Being able to safely use iPSCs without the potential of causing tumors is essential for this promising stem cell therapy to become a viable treatment option," said Stice, a Georgia Research Alliance Eminent Scholar in the College of Agricultural and Environmental Sciences. "We now have graduate students working on making neural cells from the human and pig stem cells to help further the studies. The human stem cells were effective in a rodent model for stroke, but rodent studies are not rigorous enough to start human clinical trials."
West agrees. "Over 700 drug treatments have gone to human clinical trials for stroke alone based on findings in rodents and have turned out not to be viable in humans," he said. "The pigs are much more human like, and they are going to be a much better model to study strokes."
West is leading a cooperative project between the UGA Regenerative Bioscience Center and stroke researchers at Georgia Health Sciences University. "This project will improve the speed and efficiency of treatment development for stroke and many other conditions and potentially reduce the number of nonhuman primates used in research," he said.
Additionally, Stice and West have now bred the pigs produced from iPSCs and have proven the stem cells did pass to the offspring. This finding opens the door for better animal-sourced tissue for human regenerative medicine such as islet cells that produce insulin for diabetic patients.
Using iPSC technology, the UGA Regenerative Bioscience Center is working with researchers at Emory University to make pigs whose cells from the pancreas would demonstrate decreased rejection in human treatments.
"The next step would be to put these pig insulin-producing cells into other animals, potentially dogs or cats suffering from diabetes - to see if it will produce insulin for them without being rejected," Stice said. "So, it's moving forward. Never as fast as we like, but it's moving."
Nasal Stem Cells
Nice story at http://insciences.org/article.php?article_id=9875:
Sensorineural hearing loss occurs when hearing cells in the cochlea lose their function. Frequently inherited, and usually starting during infancy and early childhood, the condition can slow a child’s development and lead to speech and language problems.
Drs Jeremy Sullivan, Sonali Pandit and Sharon Oleskevich from Sydney’s Garvan Institute of Medical Research, found that stem cells appear to release ‘factors’, or chemical substances, that help preserve the function of cochlear hearing cells, without the stem cells becoming part of the tissue of the inner ear. Their findings are published in STEM CELLS, now online.
“We are exploring the potential of stem cells to prevent or restore hearing loss in people,” said project leader Dr Sharon Oleskevich.
“The mice we are using have a very similar form of childhood deafness to their human counterparts – except, of course that mouse years are shorter. So a mouse will tend to lose their hearing within 3 months, where a person might take 8 years.”
“We are encouraged by our initial findings, because all the mice injected with stem cells showed improved hearing in comparison with those given a sham injection. Roughly half of the mice did very well indeed, although it is important to note that hearing was not completely restored to normal hearing levels.”
Adult human nasal stem cells were used in the procedure, because they are plentiful, easy to obtain and unspecialised (so have the ability to self-renew for long periods, as well as differentiate into cells with a variety of functions).
The same group of scientists has shown in previous publications that stem cells can also be used to improve hearing in noise-induced hearing loss – a condition that affects both young and older people.
It has taken 5 years to reach the current stage of research, and scientists anticipate that it will take a further decade at least for the findings to benefit people.
Acknowledgements
This research was supported by the Fairfax Foundation and the Australian Deafness Research Foundation. We received much help from ear surgeons at St. Vincent's Hospital, in particular Dr John Tonkin and Professor Paul Fagan. Also from Professor Alan Mackay-Sim, Director of the National Adult Stem Cell Research Centre at Griffith University in Brisbane, who supplied the stem cells used in the project.
Contact: Alison Heather, Science Communications Manager , Tel: +61 2 9295 8128, Email: a.heather (a) garvan.org.au
Source: The Garvan Institute of Medical Research
12/25/2011
Skeptics in Stem Cell Research
Stem cells are really promising, but it's important to be able to see all troubles that can be observed during and after the treatment.
Here is a relevant article that describes such problems:
All promises from clinics or cord blood banks should be taken with a pinch of salt, they say
With barely any regulation and monitoring in the lucrative stem cell therapy and cord blood banking business, their suggestion for the common man is to ask many questions at the clinics and companies offering such services and to fully understand the risks before going ahead with stem cell therapy and cord blood banking.
“Stem cells have lots of hopes and promises, but at the moment very few are of a proven benefit to the patients,” said Kanjaksha Ghosh, director of Mumbai’s National Institute of Immunohaematology, one of the laboratories of Indian Council of Medical Research.
Before accepting any stem cell therapy, a patient should ask whether it was an investigational or standard therapy; what the long term risks are and how many patients received it before, and what the response was, said Ghosh.
Explaining why private clinics offering stem cell therapies were mushrooming in India, Ghosh attributed the cause to the absence of strict regulation, hype about the technology and its wide availability. Also stem cell therapies are promised in desperate situations.
“Higher level of evidence is required before the stem cell therapies are put to clinical use,” Harvindersingh Chhabra at Delhi's Indian Spinal Injuries Centre said at an ICMR-department of biotechnology public consultation on stem cell.
The government in future aims at converting the revised guideline into a law on stem cell research and therapy with a punishment clause to book the doctors and clinics who flout the existing guidelines.
The misleading claims of private cord blood banks who pitch storing umbilical cord blood as “biological insurance” for lifetime protection and charge a hefty fee.
“But the volume they collect is only 70 ml, which is not sufficient if it is used to extract stem cell for anybody beyond 10 years of age,” said Shyam Agarwal, former director of Sanjay Gandhi Post Graduate Institute of Medical Education in Lucknow.
All promises from clinics or cord blood banks should be taken with a pinch of salt, they say
With barely any regulation and monitoring in the lucrative stem cell therapy and cord blood banking business, their suggestion for the common man is to ask many questions at the clinics and companies offering such services and to fully understand the risks before going ahead with stem cell therapy and cord blood banking.
“Stem cells have lots of hopes and promises, but at the moment very few are of a proven benefit to the patients,” said Kanjaksha Ghosh, director of Mumbai’s National Institute of Immunohaematology, one of the laboratories of Indian Council of Medical Research.
Before accepting any stem cell therapy, a patient should ask whether it was an investigational or standard therapy; what the long term risks are and how many patients received it before, and what the response was, said Ghosh.
Explaining why private clinics offering stem cell therapies were mushrooming in India, Ghosh attributed the cause to the absence of strict regulation, hype about the technology and its wide availability. Also stem cell therapies are promised in desperate situations.
“Higher level of evidence is required before the stem cell therapies are put to clinical use,” Harvindersingh Chhabra at Delhi's Indian Spinal Injuries Centre said at an ICMR-department of biotechnology public consultation on stem cell.
The government in future aims at converting the revised guideline into a law on stem cell research and therapy with a punishment clause to book the doctors and clinics who flout the existing guidelines.
The misleading claims of private cord blood banks who pitch storing umbilical cord blood as “biological insurance” for lifetime protection and charge a hefty fee.
“But the volume they collect is only 70 ml, which is not sufficient if it is used to extract stem cell for anybody beyond 10 years of age,” said Shyam Agarwal, former director of Sanjay Gandhi Post Graduate Institute of Medical Education in Lucknow.
A new study published in Nature reports that scientists have been able to grow working pituitary glands from embryonic stem cells from mice
The pituitary gland is a pea-sized endocrine gland at the base of the brain and secretes different hormones including Human Growth Hormone, or HGH and thyroid-stimulating hormone, or TSH. The release of these hormones plays a role in things such as growth, blood pressure, pregnancy and thyroid function. Inadequate release of certain hormones by the pituitary gland can lead to various hormone disorders.
The team of researchers, led by Dr. Yoshiki Sasai from the RIKEN Centre for Developmental Biology in Kobe, Japan has created a way to grow these little organs using embryonic stem cells from mice. Using a three dimensional culture, the team arranged the mouse stem cells in a way that mimicked the way a pituitary gland grows naturally in the embryo.
When the pituitary gland grows in the embryo, it is made from two different tissue types in the brain. Where these two different tissues come together is where the pituitary gland forms. The researchers set up the culture so these two tissues would come together similar to the way they do in the brain. The fold of tissue known as Rathke’s pouch formed naturally and grew into the pituitary gland. This pituitary gland took three weeks to grow and included all the cell types that are found in a normal pituitary gland.
The researchers then transplanted the tissue into mice that had pituitary problems and the hormone levels soon returned to normal.
While these pituitary glands were created with embryonic stem cells, the researchers believe they can use the same process successfully with stem cells taken from adults and avoid possible ethical concerns with the use of embryonic stem cells.
Research is planned to develop human pituitary glands though Sasai says that will take another four to five years. If successful, these lab-grown pituitary glands could be used to replace ones that have been damaged or do not function properly.
More information: Self-formation of functional adenohypophysis in three-dimensional culture, Nature (2011) doi:10.1038/nature10637
© 2011 PhysOrg.com
Thnx to http://medicalxpress.com/news/2011-11-pituitary-glands-embryonic-stem-cells.html for the article
The team of researchers, led by Dr. Yoshiki Sasai from the RIKEN Centre for Developmental Biology in Kobe, Japan has created a way to grow these little organs using embryonic stem cells from mice. Using a three dimensional culture, the team arranged the mouse stem cells in a way that mimicked the way a pituitary gland grows naturally in the embryo.
When the pituitary gland grows in the embryo, it is made from two different tissue types in the brain. Where these two different tissues come together is where the pituitary gland forms. The researchers set up the culture so these two tissues would come together similar to the way they do in the brain. The fold of tissue known as Rathke’s pouch formed naturally and grew into the pituitary gland. This pituitary gland took three weeks to grow and included all the cell types that are found in a normal pituitary gland.
The researchers then transplanted the tissue into mice that had pituitary problems and the hormone levels soon returned to normal.
While these pituitary glands were created with embryonic stem cells, the researchers believe they can use the same process successfully with stem cells taken from adults and avoid possible ethical concerns with the use of embryonic stem cells.
Research is planned to develop human pituitary glands though Sasai says that will take another four to five years. If successful, these lab-grown pituitary glands could be used to replace ones that have been damaged or do not function properly.
More information: Self-formation of functional adenohypophysis in three-dimensional culture, Nature (2011) doi:10.1038/nature10637
Abstract
The adenohypophysis (anterior pituitary) is a major centre for systemic hormones. At present, no efficient stem-cell culture for its generation is available, partly because of insufficient knowledge about how the pituitary primordium (Rathke’s pouch) is induced in the embryonic head ectoderm. Here we report efficient self-formation of three-dimensional adenohypophysis tissues in an aggregate culture of mouse embryonic stem (ES) cells. ES cells were stimulated to differentiate into non-neural head ectoderm and hypothalamic neuroectoderm in adjacent layers within the aggregate, and treated with hedgehog signalling. Self-organization of Rathke’s-pouch-like three-dimensional structures occurred at the interface of these two epithelia, as seen in vivo, and various endocrine cells including corticotrophs and somatotrophs were subsequently produced. The corticotrophs efficiently secreted adrenocorticotropic hormone in response to corticotrophin releasing hormone and, when grafted in vivo, these cells rescued the systemic glucocorticoid level in hypopituitary mice. Thus, functional anterior pituitary tissue self-forms in ES cell culture, recapitulating local tissue interactions.
© 2011 PhysOrg.com
Thnx to http://medicalxpress.com/news/2011-11-pituitary-glands-embryonic-stem-cells.html for the article
First. Test.
Stem cells are the most important cells in our body because they can maintain the self-renwal potential of our body.
Subscribe to:
Posts (Atom)



