That's really great idea - to make 1 minute video story about stem cells. I like it a lot:
Intro
I work with stem cells in the lab, so I want to share the information on that topic at that blog. There are lots of interesting articles and study materials about stem cells on the web that's why I'm trying to gather them all here.
Showing posts with label iPSC. Show all posts
Showing posts with label iPSC. Show all posts
9/01/2015
2/15/2013
2/07/2013
3-D printers can produce gun parts, aircraft wings, food and a lot more, but this new 3-D printed product may be the craziest thing yet: human embryonic stem cells.
Rebecca Boyle - Popular Science
3-D printers can produce gun parts, aircraft wings, food and a lot more, but this new 3-D printed product may be the craziest thing yet: human embryonic stem cells. Using stem cells as the "ink" in a 3-D printer, researchers in Scotland hope to eventually build 3-D printed organs and tissues. A team at Heriot-Watt University used a specially designed valve-based technique to deposit whole, live cells onto a surface in a specific pattern.
This article originally appeared at Popular Science.
The cells were floating in a "bio-ink," to use the terminology of the researchers who developed this technique. They were able to squeeze out tiny droplets, containing five cells or fewer per droplet, in a variety of shapes and sizes. To produce clumps of cells, the team printed out cells first and then overlaid those with cell-free bio-ink, resulting in larger droplets or spheroids of cells. The cells would group together inside these spheroids. Spheroid size is key, because stem cells need certain conditions to work properly. This is why very precisely controlled 3-D printing could be so valuable for stem cell research.
After being squeezed out of a thin valve, the cells were still alive and viable, and able to transform into any other cell in the body, the researchers say. It's the first time anyone has printed human embyronic stem cells, said lead researcher Will Wenmiao Shu, a professor at Heriot-Watt. But ... why?
Eventually, they could be used to print out new tissues, or as filler inside existing organs, which would be regenerated. It could even serve to limit animal testing for new drug compounds, allowing them to be tested on actual human tissue, said Jason King, business development manager at Roslin Cellab, one of the research partners. "In the longer term, [it could] provide organs for transplant on demand, without the need for donation and without the problems of immune suppression and potential organ rejection," he said in a statement.
The team took stem cells from an embryonic kidney and from a well-studied embryonic cell line, and grew them in culture. They had to build a custom reservoir — let's call it an inkwell — to safely house the delicate cells, and then they added some large-diameter nozzles. A pressurized air supply pumps the cells from the inkwell into the valves, which contain pressurized nozzles on the end. The team could control the amount of cells dispensed by changing any of the factors, including the pneumatic pressure, nozzle diameter or length of time the nozzle stayed open.
At first the researchers printed droplets, but ultimately, they were so precise that they made cell spheroids in a variety of shapes and sizes, like the university logo above. One interesting wrinkle: The cells also formed spheroids in the inkwells. More work needs to be done to explain that.
The researchers also took several steps to make sure the cells survived the printing process. Examining the results of several experiments, they found 99 percent of the cells were still viable after running through the valve-based printer. "This confirms that this printing process did not appear to damage the cells or affect the viability of the vast majority of dispensed cells," they write in their paper, which is being published in the IOP regenerative medicine journal Biofabrication.
Stem cells are powerful because they can develop into any cell in the body. Embryonic stem cells, which are taken from human embryos in the earliest stages of development, can be developed into stem cell lines that can be grown indefinitely. This is kind of controversial, especially in the US. But medical researchers think they could be hugely promising for a whole host of human ailments — stem cells could differentiate into neurons, potentially replacing the ones lost in degenerative diseases like Alzheimer's; or they could differentiate into pancreatic cells, curing diabetes; and so on.
Using a 3-D printer to produce gun parts has been pretty controversial, especially during the ongoing post-Connecticut-shooting gun debate. But that may be nothing compared to this.
http://io9.com/5981832/a-3d-printer-that-generates-human-embryonic-stem-cells
3-D printers can produce gun parts, aircraft wings, food and a lot more, but this new 3-D printed product may be the craziest thing yet: human embryonic stem cells. Using stem cells as the "ink" in a 3-D printer, researchers in Scotland hope to eventually build 3-D printed organs and tissues. A team at Heriot-Watt University used a specially designed valve-based technique to deposit whole, live cells onto a surface in a specific pattern.
This article originally appeared at Popular Science.
The cells were floating in a "bio-ink," to use the terminology of the researchers who developed this technique. They were able to squeeze out tiny droplets, containing five cells or fewer per droplet, in a variety of shapes and sizes. To produce clumps of cells, the team printed out cells first and then overlaid those with cell-free bio-ink, resulting in larger droplets or spheroids of cells. The cells would group together inside these spheroids. Spheroid size is key, because stem cells need certain conditions to work properly. This is why very precisely controlled 3-D printing could be so valuable for stem cell research.
After being squeezed out of a thin valve, the cells were still alive and viable, and able to transform into any other cell in the body, the researchers say. It's the first time anyone has printed human embyronic stem cells, said lead researcher Will Wenmiao Shu, a professor at Heriot-Watt. But ... why?
Eventually, they could be used to print out new tissues, or as filler inside existing organs, which would be regenerated. It could even serve to limit animal testing for new drug compounds, allowing them to be tested on actual human tissue, said Jason King, business development manager at Roslin Cellab, one of the research partners. "In the longer term, [it could] provide organs for transplant on demand, without the need for donation and without the problems of immune suppression and potential organ rejection," he said in a statement.
The team took stem cells from an embryonic kidney and from a well-studied embryonic cell line, and grew them in culture. They had to build a custom reservoir — let's call it an inkwell — to safely house the delicate cells, and then they added some large-diameter nozzles. A pressurized air supply pumps the cells from the inkwell into the valves, which contain pressurized nozzles on the end. The team could control the amount of cells dispensed by changing any of the factors, including the pneumatic pressure, nozzle diameter or length of time the nozzle stayed open.
At first the researchers printed droplets, but ultimately, they were so precise that they made cell spheroids in a variety of shapes and sizes, like the university logo above. One interesting wrinkle: The cells also formed spheroids in the inkwells. More work needs to be done to explain that.
The researchers also took several steps to make sure the cells survived the printing process. Examining the results of several experiments, they found 99 percent of the cells were still viable after running through the valve-based printer. "This confirms that this printing process did not appear to damage the cells or affect the viability of the vast majority of dispensed cells," they write in their paper, which is being published in the IOP regenerative medicine journal Biofabrication.
Stem cells are powerful because they can develop into any cell in the body. Embryonic stem cells, which are taken from human embryos in the earliest stages of development, can be developed into stem cell lines that can be grown indefinitely. This is kind of controversial, especially in the US. But medical researchers think they could be hugely promising for a whole host of human ailments — stem cells could differentiate into neurons, potentially replacing the ones lost in degenerative diseases like Alzheimer's; or they could differentiate into pancreatic cells, curing diabetes; and so on.
Using a 3-D printer to produce gun parts has been pretty controversial, especially during the ongoing post-Connecticut-shooting gun debate. But that may be nothing compared to this.
http://io9.com/5981832/a-3d-printer-that-generates-human-embryonic-stem-cells
9/02/2012
Another one stem cell fraud
Wired news... Stem cell research becomes a strange place... Here's some recent events:
http://retractionwatch.wordpress.com/2012/08/29/ori-finds-harvard-stem-cell-lab-post-doc-mayack-manipulated-images/
Shane Mayack, a former post-doc in Harvard lab of Amy Wagers, a rising star in the stem cell field, has been sanctioned by the Office of Research Integrity for misconduct.
Mayack, who has defended her actions on this blog as honest error — albeit sloppiness — and has not admitted to wrongdoing, must undergo supervision if she receives any federal grant funding over the next three years, under the voluntary agreement.
Here’s the notice, which appeared in the Federal Register this week (and which theBoston Globe was first to report):
Based on the report of an investigation conducted by the Joslin Diabetes Center (Joslin) and additional analysis conducted by ORI in its oversight review, ORI found that Dr. Shane Mayack, former postdoctoral fellow, Department of Developmental and Stem Cell Biology, Joslin, engaged in research misconduct in research supported by National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (NIH), grants T32 DK07260–29 and P30 DK036836 and the 2008 NIH Director’s New Innovator Award Program grant DP2 OD004345–01.
ORI found that Respondent engaged in research misconduct involving two (2) published papers:
• Mayack, S.R., Shadrach, J.L., Kim, F.S., & Wagers, A.J. ‘‘Systemic signals regulate ageing and rejuventation of blood stem cell niches.’’ Nature 463:495–500, 2010.
• Mayack, S.R., & Wagers, A.J. ‘‘Osteolineage niche cells initiate hemotopoietic stem cell mobilization.’’ Blood 112:519–531, 2008.
As a result of Joslin’s investigation, both Nature 463:495–500, 2010 (hereafter referred to as the ‘‘Nature paper’’) and Blood 112:519–531, 2008 (hereafter referred to as the ‘‘Blood paper’’) have been retracted by the corresponding author.
Specifically, ORI found that:
• Respondent falsely represented von Kossa-stained bone nodule images in two (2) published papers:
Figure 2B in the Blood paper was copied from an unrelated published experiment in Figure 3, J Orth Surg Res 1:7, 2006, and was used to falsely represent Respondent’s own experiment for bone nodules formed in cultured osteoblastic niche cells.
b. Figure S2c in the Nature paper was copied from an online image for an unrelated experiment (at http://skeletalbiology.uchc.edu/30_ResearchProgram/304_gap/3042_Lineage%20in%20Vitro/3042_01_aCellCult.htm#mCOB) and was used to falsely represent Respondent’s own experiment for bone nodules formed in osteoblastic niche cells from young and aged mice.
• Respondent falsely represented eight (8) flow cytometry contour plots as different experimental results by using identical plots but with different labels and different numerical percentages.
Specifically, the following contour plots in the Blood paper, the Nature paper, an earlier version of the Nature paper submitted to Science (hereafter referred to as the ‘‘Science manuscript’’), and a July 2008 PowerPoint presentation were identical but were labeled differently:
a. Panels 4 and 2 in Figure 6C, Blood paper, and panels 1 and 2, respectively, in supplementary Figure 3b, Nature paper
b. Panel 3 in Figure 6C, Blood paper, and panel 1 in Figure 2, July 2008 PowerPoint presentation
Panels 1 and 2, Figure 2b, Science manuscript, and panels 2 and 3, respectively, in Figure 2, July 2008 PowerPoint presentation
Panels 2, 3, and 4, supplemental Figure 4A, Blood paper, and panels 3, 1, and 2, respectively, in Figure 4B, Science manuscript
Both the Respondent and HHS want to conclude this matter without further expenditure of time or other resources and have entered into a Voluntary Settlement Agreement to resolve this matter. Respondent neither admits nor denies ORI’s finding of research misconduct. This settlement does not constitute an admission of liability on the part of the Respondent.
Nearly two years have passed since we first wrote about Mayack. At the time, Wagers’ group had just retracted a 2010 Nature paper — with a notable exception: Mayack refused to sign the notice, nor did she sign the notice for the retraction of the Blood paper, which appeared in late 2011.
As she wrote on this blog:
… the readers of Retraction Watch are no doubt aware that in October 2010, a paper that I co-authored was retracted fromNature and a notice of concern was posted regarding a second paper published in Blood.
So, what went wrong?
The answer to that question begins with the fact that errors, not fabrications, were made in assembling figures for these manuscripts. I am likely the one who made these errors.
Mayack reiterated that position in a comment, through her attorney, to us today:
I remain deeply sorry to the scientific community for mistakes made during the preparation of figures corresponding to some of the work I performed as a postdoc at Harvard Medical School. These were mistakes in representation and presentation of the data, as corroborated by ORI’s findings of ‘falsely presented’, and were not due to fabrication, falsification, or plagiarism of scientific results. I am deeply committed to moving forward and strive to contribute positively to the advancement of science, which has always been my utmost interest.
Wagers recently received tenure.
http://retractionwatch.wordpress.com/2012/08/29/ori-finds-harvard-stem-cell-lab-post-doc-mayack-manipulated-images/
8/27/2012
.
Here is the express Stem Cell news on the other place - my paper.li. Very interesting place to put your information. I like it!:
6/08/2012
5/29/2012
...antipsychotic drug, Thioridazine, has activity against cancer stem cells
Mick Bhatia’s lab has found that the antipsychotic drug, Thioridazine, has activity against cancer stem cells.
The work, published in Cell (read paper here), indicates that Thioridazine works not by killing cancer stem cells, but rather by encouraging the stem cells to differentiate.
Bhatia’s group used a novel screening approach (see graphical abstract from the paper above) to find molecules that specifically differentiate cancer stem cells. Interestingly they found Thioridazine, which intriguingly targets the dopamine receptor expressed on certain cancer stem cells. Bhatia can be seen in the interview below talking about the finding.
You might think then that Thioridazine would be safe because it only targets cells expressing dopamine receptor, however the drug reportedly has significant safety concerns due to causing fatal heart arrhythmias and regulators have largely phased it out in both Canada and the U.S..
Even so, it may be safe for cancer treatments since it could be used for a much shorter period of time, speculated Bhatia. However it is still early days in this story so there is much to learn about this new route to attacking cancer. Still, a very exciting and important development.
Thanks to https://www.ipscell.com/2012/05/psyching-out-cancer-stem-cells-using-old-antipsychotic-drug-as-a-new-weapon-against-cancer/ for the information.
5/26/2012
Stem Cell Comics
Open publication - Free publishing
Beautiful educational comics about stem cells! ‘Hope Beyond Hype’ is a story about stem cell therapies from science discovery to working therapy.
4/16/2012
Cool Article About the History of Stem Cell Research!
That's wonderful! I thought about it lots of times!
Who really discovered stem cells?
Is it even possible that one scientific team all by themselves discovered something so ubiquitous as stem cells?
In theory “yes”, but after much historical research including this great historical article in Cell Stem Cell, I would argue that no one group really discovered stem cells.
Instead I believe the “discovery” of stem cells was an ongoing team effort over a period of many decades and there is much credit to go around.
Who gets the credit now according to most people now for “discovering” stem cells?
Canada rightly takes pride in the work of their scientists Drs. James Till and Ernset McCulloch, who did pioneering studies in hematopoietic stem cell research.
In Canada, Till and McCulloch are unambiguously called the world’s discoverers of stem cells. Period. No ambiguity.
But is that correct?
Nope.
2/24/2012
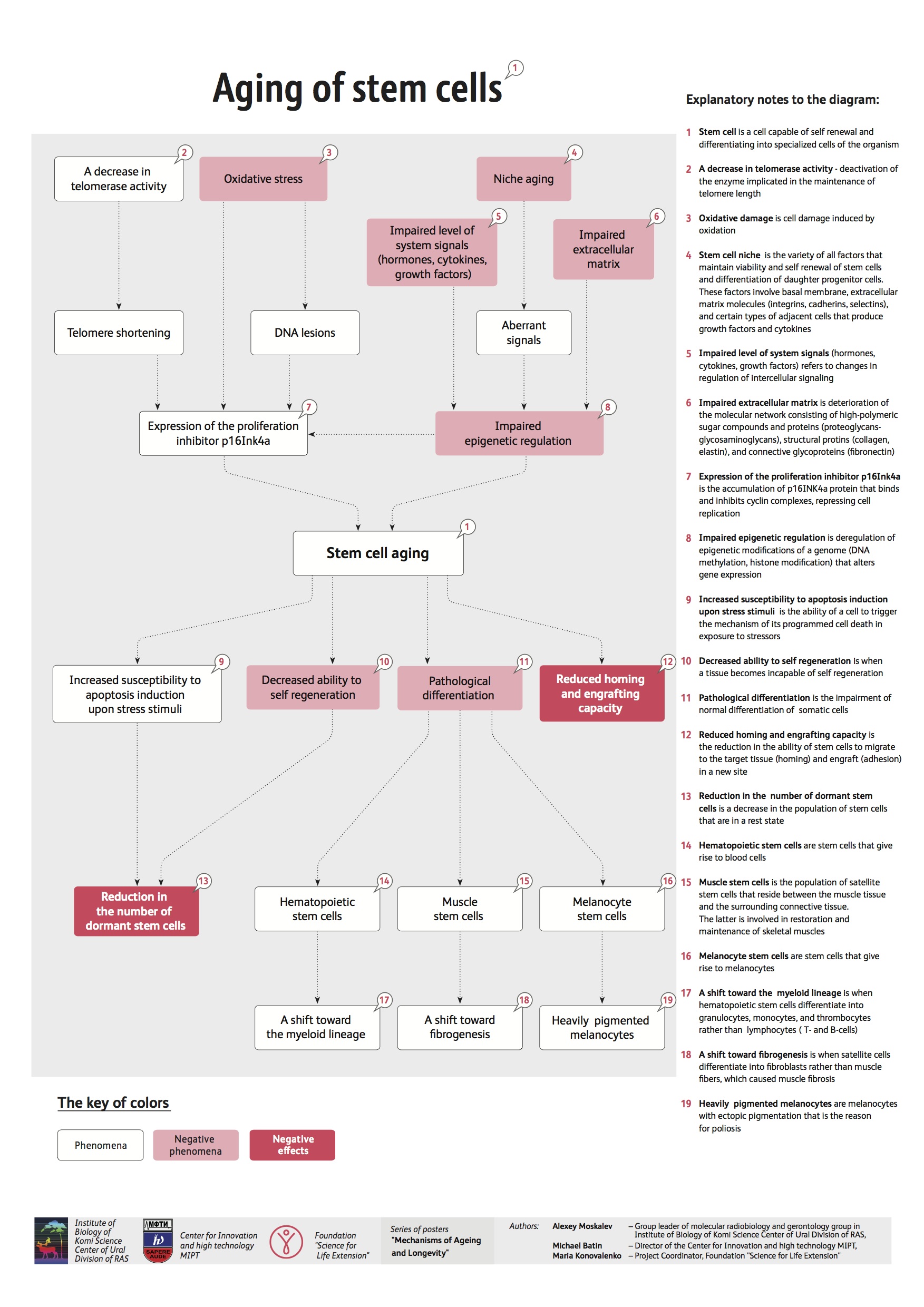
Stem Cell Aging
http://www.fightaging.org/images/aging_of_stem_cells.jpg
the problem of Stem Cell Aging is one of the most intrigueing in stem cell biology field.
1/12/2012
Stem Cells & Future Medicine (important opinion)
I'd like to share an interesting opinion from Sara Rankin, Professor of Leukocyte and Stem Cell Biology at Imperial College London's Faculty of Medicine, turns the spotlight onto the future impact of stem cell therapy:
Canadian scientists investigating the effects of radiation on the human body 50 years ago discovered that bone marrow 1contains stem cells that provide a lifelong supply of blood cells. This discovery paved the way for the first stem cell therapy – in the form of bone marrow transplants – using bone marrow stem cells from healthy donors to treat patients with genetic blood disorders and leukaemias.
Scientists went on to show that in addition to the bone marrow, almost every tissue in the body, including heart, brain, teeth and gut, contain tissue-specific stem cells. The function of these stem cells is to repair or regenerate tissues that are constantly being damaged as a result of general wear and tear – for example, replacing the lining of the gut as it is being sloughed off or generating new blood cells as they die or are destroyed. Such tissue-specific stem cells are also known as adult stem cells, simply because they are found in adult tissues. These adult stem cells are distinct from embryonic (ES) stem cells that are only found in embryos.
Canadian scientists investigating the effects of radiation on the human body 50 years ago discovered that bone marrow 1contains stem cells that provide a lifelong supply of blood cells. This discovery paved the way for the first stem cell therapy – in the form of bone marrow transplants – using bone marrow stem cells from healthy donors to treat patients with genetic blood disorders and leukaemias.
Scientists went on to show that in addition to the bone marrow, almost every tissue in the body, including heart, brain, teeth and gut, contain tissue-specific stem cells. The function of these stem cells is to repair or regenerate tissues that are constantly being damaged as a result of general wear and tear – for example, replacing the lining of the gut as it is being sloughed off or generating new blood cells as they die or are destroyed. Such tissue-specific stem cells are also known as adult stem cells, simply because they are found in adult tissues. These adult stem cells are distinct from embryonic (ES) stem cells that are only found in embryos.
1/10/2012
1/09/2012
Education (stem cell topic)
Beautiful stem cell education resource: http://www.tellmeaboutstemcells.org/
1/06/2012
Stemmy!111 ^_^
So cuuuuute!11111
And more about Stemmy:
Aaaaaannnnnddddd moooooooreeee:
And more about Stemmy:
Aaaaaannnnnddddd moooooooreeee:
Pictures from http://www.terry.ubc.ca/2009/08/07/faq-stem-cells-sa-mix/, moreover you can find text there.
12/29/2011
12/27/2011
Stem Cells!
Beautiful Stem Cells! Thnx to
http://stemcelldaily.com/stem-cells-are-purdy-pics/ :

Neurosphere composed of neural precursor cells as captured by a fluorescent microscope. The cells, allowed to attach to a substrate, have begun to send out long processes that will eventually become the axons of the mature neurons.
The image was taken in the lab of Martin Pera at the University of Southern California.

A confocal microscopic image of a neurosphere, a ball of human embryonic stem cells giving rise to nerve cells. The nuclei of the neurons are shown in blue, while the axons are shown in red.
The image was taken in the lab of Juan Carlos Izpisua Belmonte at The Salk Institute for Biological Studies.

Color-enhanced electron microscopic image of mouse embryonic stem cells growing on a bed of silicon nanotubes.
The image was taken in the lab of Bruce Conklin at the Gladstone Institute for Cardiovascular Medicine.

Color-enhanced image taken by a scanning electron microscope of retinal pigment epithelial (RPE) cells derived from human embryonic stem cells. The cells are remarkably similar to normal RPE cells, having a hexagonal shape and growing in a single, well defined layer. These cells are the ones responsible for macular degeneration, the most common cause of blindness. CIRM scientists hope to one day treat macular degeneration with transplanted RPE cells derived from human embryonic stem cells.
The image was taken in the lab of David Hinton at the University of Southern California.
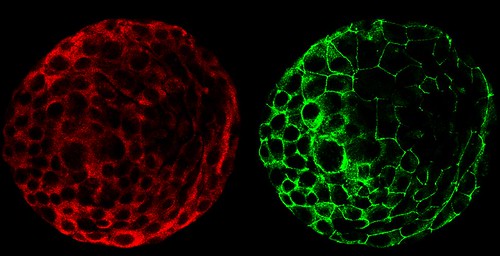

A composite of two images taken of a human embryo under different fluorescent wavelengths using a confocal microscope.
Fluorescent tags reveal that cells on the surface of the embryo are expressing human chorinoic gonadotropin (green tag) and an adhesion molecule (red tag)that helps them stick together.
The image was taken in the lab of Susan Fisher at the University of California, San Francisco.

A fluorescent microscopic image of hundreds of human embryonic stem cells in various stages of differentiation into neurons. Some cells have become neurons (red), while others are still precursors of nerve cells (green). The yellow is an imaging artifact that results when cells in both stages are on top of each other.
The image was taken in the lab of Guoping Fan at the University of California, Los Angeles.

Colonies of human embryonic stem cells as seen with a fluorescent microscope. Nuclei have been stained blue, while regions that appear pink and green have been stained with antibodies, indicating the cells’ pluripotency — that unique ability of stem cells to differentiate into a variety of cell types.
The image was taken in the lab of Prue Talbot at the University of California, Riverside.


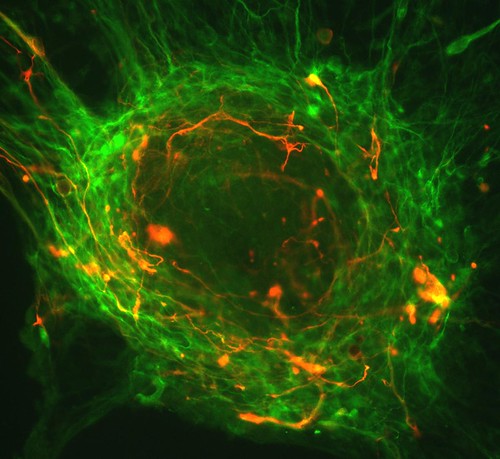
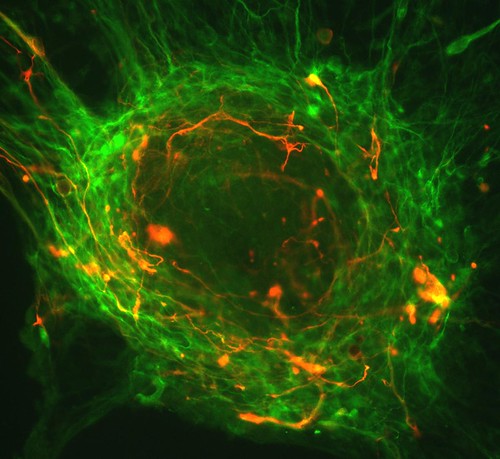
Three neurons (red) derived from human embryonic stem cells (hESCs) as seen by a confocal microscope. Visible are neural cell bodies, complete with axons and dendrites (red), used for cell-to-cell communications, as well as undifferentiated hESCs (green).
The image was taken in the lab of Anirvan Ghosh at the University of California, San Diego.


A fluorescent microscopic image of a functional neuron with an axon (red) growing above the cell’s nucleus and three dendrites (red) below. Undifferentiated neural precursor cells (blue) are visible as are glia cells (green) that have differentiated from the same group of mouse neural stem cells.
The image was taken in the lab of Paul Knoepfler at the University of California, Davis.


Two neurospheres, compact masses of neuron precursor cells, derived from human embryonic stem cells, as captured by a fluorescent microscope. Differentiated neurons, whose nuclei are shown in red, have begun to extend neuronal processes (green) toward one another, forming connections.

Neurosphere composed of neural precursor cells as captured by a fluorescent microscope. The cells, allowed to attach to a substrate, have begun to send out long processes that will eventually become the axons of the mature neurons.
The image was taken in the lab of Martin Pera at the University of Southern California.

A confocal microscopic image of a neurosphere, a ball of human embryonic stem cells giving rise to nerve cells. The nuclei of the neurons are shown in blue, while the axons are shown in red.
The image was taken in the lab of Juan Carlos Izpisua Belmonte at The Salk Institute for Biological Studies.

Color-enhanced electron microscopic image of mouse embryonic stem cells growing on a bed of silicon nanotubes.
The image was taken in the lab of Bruce Conklin at the Gladstone Institute for Cardiovascular Medicine.

Color-enhanced image taken by a scanning electron microscope of retinal pigment epithelial (RPE) cells derived from human embryonic stem cells. The cells are remarkably similar to normal RPE cells, having a hexagonal shape and growing in a single, well defined layer. These cells are the ones responsible for macular degeneration, the most common cause of blindness. CIRM scientists hope to one day treat macular degeneration with transplanted RPE cells derived from human embryonic stem cells.
The image was taken in the lab of David Hinton at the University of Southern California.
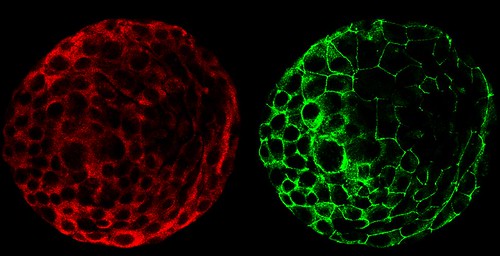

A composite of two images taken of a human embryo under different fluorescent wavelengths using a confocal microscope.
Fluorescent tags reveal that cells on the surface of the embryo are expressing human chorinoic gonadotropin (green tag) and an adhesion molecule (red tag)that helps them stick together.
The image was taken in the lab of Susan Fisher at the University of California, San Francisco.

A fluorescent microscopic image of hundreds of human embryonic stem cells in various stages of differentiation into neurons. Some cells have become neurons (red), while others are still precursors of nerve cells (green). The yellow is an imaging artifact that results when cells in both stages are on top of each other.
The image was taken in the lab of Guoping Fan at the University of California, Los Angeles.

Colonies of human embryonic stem cells as seen with a fluorescent microscope. Nuclei have been stained blue, while regions that appear pink and green have been stained with antibodies, indicating the cells’ pluripotency — that unique ability of stem cells to differentiate into a variety of cell types.
The image was taken in the lab of Prue Talbot at the University of California, Riverside.


Three neurons (red) derived from human embryonic stem cells (hESCs) as seen by a confocal microscope. Visible are neural cell bodies, complete with axons and dendrites (red), used for cell-to-cell communications, as well as undifferentiated hESCs (green).
The image was taken in the lab of Anirvan Ghosh at the University of California, San Diego.


A fluorescent microscopic image of a functional neuron with an axon (red) growing above the cell’s nucleus and three dendrites (red) below. Undifferentiated neural precursor cells (blue) are visible as are glia cells (green) that have differentiated from the same group of mouse neural stem cells.
The image was taken in the lab of Paul Knoepfler at the University of California, Davis.


Two neurospheres, compact masses of neuron precursor cells, derived from human embryonic stem cells, as captured by a fluorescent microscope. Differentiated neurons, whose nuclei are shown in red, have begun to extend neuronal processes (green) toward one another, forming connections.
The image was taken in the lab of Fred H. Gage at the Salk Institute for Biological Studies.

Neurospheres made up of neural stem cells derived from human embryonic stem cells captured using fluorescence microscopy. Some cells (green) are destined to become neurons; others have yet to differentiate (red) or are in transition (yellow).
This photo was taken in the lab of Brian Cummings at the University of California, Irvine.

A composite image of frames taken of a developing human embryo captured using time-lapse video microscopy and a phase contrast microscope. The earliest frame is of a three-day-old embryo and appears in the upper left corner. An image of a five-day-old embryo appears in the lower right.
This photo was taken in the lab of Susan Fisher at the University of California, San Francisco.
You can find out more information about the contest here.

Neurospheres made up of neural stem cells derived from human embryonic stem cells captured using fluorescence microscopy. Some cells (green) are destined to become neurons; others have yet to differentiate (red) or are in transition (yellow).
This photo was taken in the lab of Brian Cummings at the University of California, Irvine.

A composite image of frames taken of a developing human embryo captured using time-lapse video microscopy and a phase contrast microscope. The earliest frame is of a three-day-old embryo and appears in the upper left corner. An image of a five-day-old embryo appears in the lower right.
This photo was taken in the lab of Susan Fisher at the University of California, San Francisco.
You can find out more information about the contest here.
12/26/2011
Pigs are our friends :)
Pig stem cell research conducted by two animal scientists at the University of Georgia reveals a better way to determine the safety of future stem cell therapies than rodent-based models.
Rodent studies are likely inadequate for testing many human therapies - including pharmaceuticals - since 50 percent of all chemicals test positive as carcinogens in rodents regardless of their source or identity, according to Thomas Hartung, a professor in the Bloomsburg College of Public Health at Johns Hopkins University. He suggests these rodent studies may be no better than a coin toss. For example, some components in coffee appear to be carcinogenic in rodents, but in humans moderate coffee consumption may reduce the risk of cancer.
In 2010, UGA faculty Steve Stice and Franklin West introduced 13 pigs that have shown promise in unlocking the path to new therapies. The pigs recently produced another positive finding: These adult-cell-sourced stem cells don't form tumors in pigs.
"Pluripotent stem cells have significant potential for stem cell therapies," said West, an animal science researcher and assistant professor in the UGA College of Agricultural and Environmental Sciences. "However, tests in mice often resulted in tumor formation that frequently led to death."
The formation of tumors has raised concerns about the safety of induced pluripotent stem cells, or iPSCs, and cells derived from these stem cells. Until now, all iPSC safety studies have been performed in rodent models.
"To address the concern, our research team studied tumor formation in pigs generated from pig iPSCs," West said. "Brain, skin, liver, pancreas, stomach, intestine, lung, heart, kidney, muscle, spleen and gonad tissues from all 11 pigs tested showed no evidence of tumors."
The absence of tumor formation in these pigs suggests that iPSCs can safely incorporate into tissues without tumor formation.
"Being able to safely use iPSCs without the potential of causing tumors is essential for this promising stem cell therapy to become a viable treatment option," said Stice, a Georgia Research Alliance Eminent Scholar in the College of Agricultural and Environmental Sciences. "We now have graduate students working on making neural cells from the human and pig stem cells to help further the studies. The human stem cells were effective in a rodent model for stroke, but rodent studies are not rigorous enough to start human clinical trials."
West agrees. "Over 700 drug treatments have gone to human clinical trials for stroke alone based on findings in rodents and have turned out not to be viable in humans," he said. "The pigs are much more human like, and they are going to be a much better model to study strokes."
West is leading a cooperative project between the UGA Regenerative Bioscience Center and stroke researchers at Georgia Health Sciences University. "This project will improve the speed and efficiency of treatment development for stroke and many other conditions and potentially reduce the number of nonhuman primates used in research," he said.
Additionally, Stice and West have now bred the pigs produced from iPSCs and have proven the stem cells did pass to the offspring. This finding opens the door for better animal-sourced tissue for human regenerative medicine such as islet cells that produce insulin for diabetic patients.
Using iPSC technology, the UGA Regenerative Bioscience Center is working with researchers at Emory University to make pigs whose cells from the pancreas would demonstrate decreased rejection in human treatments.
"The next step would be to put these pig insulin-producing cells into other animals, potentially dogs or cats suffering from diabetes - to see if it will produce insulin for them without being rejected," Stice said. "So, it's moving forward. Never as fast as we like, but it's moving."
Rodent studies are likely inadequate for testing many human therapies - including pharmaceuticals - since 50 percent of all chemicals test positive as carcinogens in rodents regardless of their source or identity, according to Thomas Hartung, a professor in the Bloomsburg College of Public Health at Johns Hopkins University. He suggests these rodent studies may be no better than a coin toss. For example, some components in coffee appear to be carcinogenic in rodents, but in humans moderate coffee consumption may reduce the risk of cancer.
In 2010, UGA faculty Steve Stice and Franklin West introduced 13 pigs that have shown promise in unlocking the path to new therapies. The pigs recently produced another positive finding: These adult-cell-sourced stem cells don't form tumors in pigs.
"Pluripotent stem cells have significant potential for stem cell therapies," said West, an animal science researcher and assistant professor in the UGA College of Agricultural and Environmental Sciences. "However, tests in mice often resulted in tumor formation that frequently led to death."
The formation of tumors has raised concerns about the safety of induced pluripotent stem cells, or iPSCs, and cells derived from these stem cells. Until now, all iPSC safety studies have been performed in rodent models.
"To address the concern, our research team studied tumor formation in pigs generated from pig iPSCs," West said. "Brain, skin, liver, pancreas, stomach, intestine, lung, heart, kidney, muscle, spleen and gonad tissues from all 11 pigs tested showed no evidence of tumors."
The absence of tumor formation in these pigs suggests that iPSCs can safely incorporate into tissues without tumor formation.
"Being able to safely use iPSCs without the potential of causing tumors is essential for this promising stem cell therapy to become a viable treatment option," said Stice, a Georgia Research Alliance Eminent Scholar in the College of Agricultural and Environmental Sciences. "We now have graduate students working on making neural cells from the human and pig stem cells to help further the studies. The human stem cells were effective in a rodent model for stroke, but rodent studies are not rigorous enough to start human clinical trials."
West agrees. "Over 700 drug treatments have gone to human clinical trials for stroke alone based on findings in rodents and have turned out not to be viable in humans," he said. "The pigs are much more human like, and they are going to be a much better model to study strokes."
West is leading a cooperative project between the UGA Regenerative Bioscience Center and stroke researchers at Georgia Health Sciences University. "This project will improve the speed and efficiency of treatment development for stroke and many other conditions and potentially reduce the number of nonhuman primates used in research," he said.
Additionally, Stice and West have now bred the pigs produced from iPSCs and have proven the stem cells did pass to the offspring. This finding opens the door for better animal-sourced tissue for human regenerative medicine such as islet cells that produce insulin for diabetic patients.
Using iPSC technology, the UGA Regenerative Bioscience Center is working with researchers at Emory University to make pigs whose cells from the pancreas would demonstrate decreased rejection in human treatments.
"The next step would be to put these pig insulin-producing cells into other animals, potentially dogs or cats suffering from diabetes - to see if it will produce insulin for them without being rejected," Stice said. "So, it's moving forward. Never as fast as we like, but it's moving."
Subscribe to:
Posts (Atom)